
Newborn Assessment
INITIAL RAPID ASSESSMENT OF NEWBORN
This module focuses on assessment of the newborn infant. The assessment begins at birth and is done periodically by the nurse during the next two to four days. This eLearning module will describe assessment techniques and normal variations in newborn appearance.
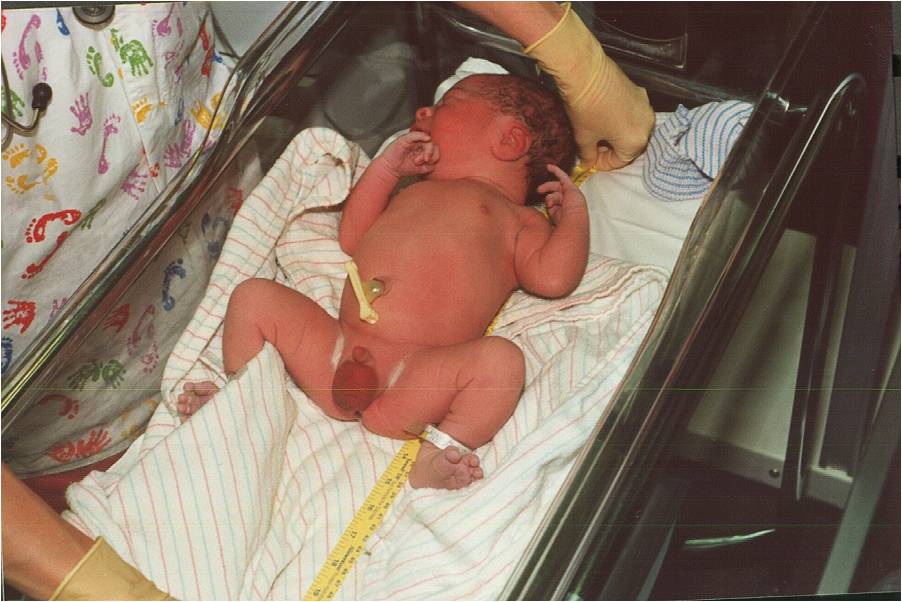
After the infant is born, your initial assessment is quick and will occur at the same time you are drying and warming the infant for placement on the mother's chest for skin-to-skin contact or under the warmer. Don't forget to wear gloves until after the infant has been bathed. The infant is wet with amniotic fluid and slippery and may be a bit bloody.

Your initial assessment is primarily listening and observation.

This infant shows little muscle tone of arms and legs.

Picture used with permission Dr. Janelle Aby, Stanford Medical School, Palo Alto, CA
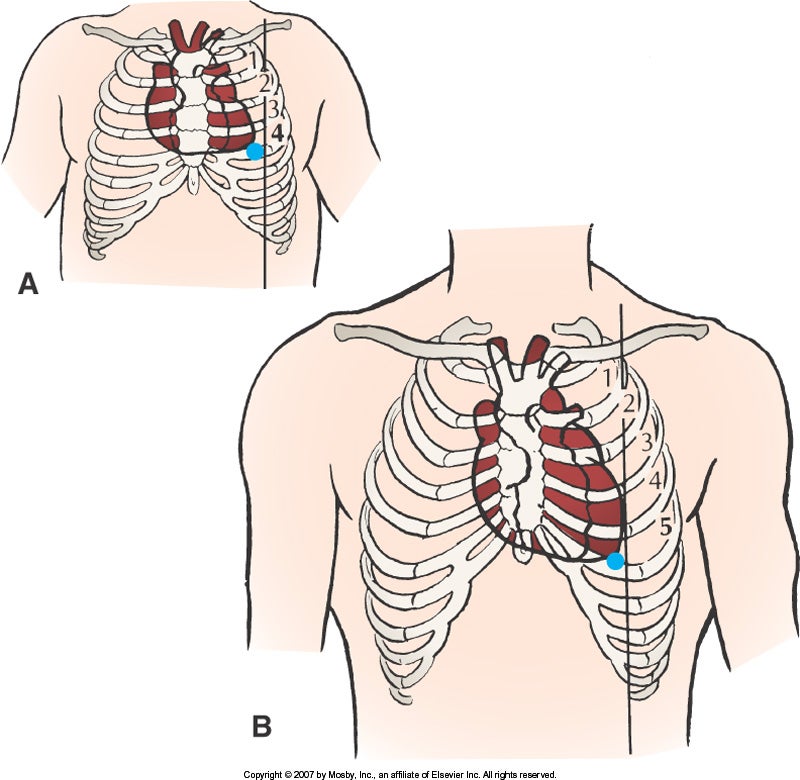
This infant shows substernal retractions and intercostal retractions. These are signs of respiratory distress.
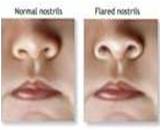
Left picture is normal.
Right picture shows nasal flaring. This can be a sign of respiratory distress.
APGAR SCORE
|
SCORE |
0 |
1 |
2 |
|
Appearance (Skin color) |
Blue or Pale |
Body pink; hands and feet blue |
Completely pink |
|
Pulse (Heart Rate) |
Absent |
< 100 beats per minute |
> 100 beats per minute |
|
Grimace (Reflex Irritability) |
Absent |
Grimace |
Grimace (or vigorous cry) and cough or sneeze |
|
Activity (Muscle Tone) |
Limp |
Some flexing of arms and legs |
Active flexing of arms and legs; active motion |
|
Respiration |
Absent |
Slow, irregular respirations; weak cry |
Good respirations (30-60): strong cry |

Healthy Response to Birth
|
|
|
|
Mother and infant, skin-to-skin |
Dad and infant, skin-to-skin |
At Risk Response to Birth
VITAL SIGNS
Vital signs for the infant include heart rate, respirations and temperature. Initially the vital signs are monitored every half hour for the first two hours after birth. After stabilization, newborn assessments including vital signs occur every four to eight hours.
It is easiest to assess the heart rate and respirations while the infant is quiet. If the infant is crying, you may try to calm the infant by wrapping and rocking the infant. You may also insert a clean, gloved finger into the infant's mouth. The infant's suck will be initiated and the infant will quiet.
Heart Rate
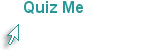
Auscultate the apical heart rate at the border of the left sternum for a full minute.
Note: The PMI of the infant's heart is lateral to the midclavicular line at the left lower sternal border at the 4th ICS whereas the adult's PMI is at the 5th ICS (see pictue on the right).

Picture used with permission Dr. Janelle Aby, Stanford Medical School, Palo Alto, CA Elsevier
The infant's normal heart rate is 120-160 beats per minute and irregular. During sleep the heart rate may decrease to 100. After birth or while crying, the heart rate may be as high as 180. If you have difficulty counting the heart rate, tap your finger or foot with each beat. Be patient. Counting a newborn's heart rate for a minute takes PRACTICE. After you have counted for a minute, move to each of the four areas of the heart to listen for a heart murmur or heart irregularities.
Respirations
During inspirations observe the bilateral expansion of the barrel-shaped chest. Observe for symmetry and retractions.

Left: Normal nares vs. nasal flaring Right:Intracostal retractions
Observe for signs of respiratory distress which include: nasal flaring, intercostal retractions between the ribs, or a grunting or a singing noise with inspiration.
Count the respiratory rate for a full minute. You may want to observe the rise and fall of the abdomen as you count the respirations. The respiratory rate is irregular due to the immature neurological system. The best position to listen is the opposite side from the heart. The normal rate is 30 to 60 breaths per minute. A respiratory rate that is tachypneic or bradypneic two hours after delivery may indicate a problem. Listen to bilateral breath sounds from the base (bottom) of the lungs to the apex (top) of the lungs with the infant lying on his/her back. Note the presence of crackles or wheezes.
Although not a part of the vital signs, assess the abdomen. Observe the soft, dome-shaped, round abdomen which moves with respirations. Listen to the four quadrants for bowel sounds. You may now put aside your stethoscope. Usually the abdomen is not palpated.
Temperature
The axillary temperature is taken by inserting the digital thermometer under the axilla in line with the infant's arm. Hold the infant's arm firmly against the thermometer. The infant may cry. Be patient. It will be over soon.

The normal axillary temperature is 36.5 to 37.2 C. Due to wetness after birth and lack of body fat, infants are at risk for hypothermia. The infant should be uncovered for a very short period of time. The infant hat maintains body warmth. The first bath is not given until the infant has three temperatures above 36.5 C. The axillary temperature is the method of choice until age 6.
Note: The heart rate, respirations and temperature can be completed when the infant is held skin-to-skin by the mother. The stable infant does not need to return to the radiant warmer for assessments. It is always important to complete the assessments rapidly to prevent hypothermia.
Inability to maintain temperature (inadequate thermoregulation) can be the first sign of infection or sepsis for the infant. In addition to a temperature less than 36.5 C, other signs of infection may include rapid respirations and inadequate feeding. Note that infants may have a low temperature whereas adults have an elevated temperature with infection.
A more complete head-to-toe examination follows the initial rapid assessment and vital signs. It may be delayed until the mother has breastfed her infant or held the infant skin-to-skin.
Test your memory...
WEIGHT, HEAD AND CHEST CIRCUMFERENCE AND LENGTH
The weight, head and chest circumference and length are measured soon after birth. These may be delayed so that the mother and infant may bond with skin-to-skin contact.
Weight
The initial weight is measured soon after birth. Place a protective paper on the sanitized digital scale and set it to "0". The infant is placed on the scale without clothing. Keep gloved hands close to the infant to prevent a fall. Note weight in kilograms and pounds. Weigh the infant quickly to prevent heat loss, which could lead to hypothermia.

An infant born at 40 weeks gestation (normal pregnancy) and weighing >2500 grams and < 4000 grams is considered AGA or appropriate for gestational age. A small infant is SGA. A large infant is LGA. Although infants can lose up to 10% of their birth weight during the first few days, the physician should be notified if the infant loses 7% of birth weight to monitor for dehydration. The lost weight is regained within the first two weeks. Weight is obtained daily at the same time. SGA and LGA infants are at risk for hypoglycemia. Their glucose levels will be monitored closely in the first few hours after birth.
|
|
|
|
|
AGA: 7 Lb |
SGA: 5 Lb 7 OZ |
LGA: 8 Lb 9 Oz |
Pictures used with permission from Dr. Janelle Aby, Stanford Medical Center, Palo Alto,CA
Head Circumference (FOC or frontal occipital circumference)
A clean paper tape is used for each infant. Usually it is located in the "newborn pack" that includes hats, shampoo and comb. Measure the head circumference at the greatest diameter around the forehead (frontal area) and back of head (occiput). The average head circumference (HC) is 33-37 cm.

Microcephaly (as in the picture below) is a head smaller than 32 cm. Hydrocephalus occurs when the head is 4 cm greater than chest circumference.

Picture used with permission Dr. Janelle Aby, Stanford Medical School, Palo Alto, CA
Chest Circumference
Measure the chest circumference at the nipple line. The average is 30 to 33 cm and should be 2-3 cm LESS THAN head circumference.

Elsevier picture (Courtesty Marjorie Pyle, RNC, Lifecircle, Costa Mesa, CA).
Length
Measure from the top of the head to the bottom of the heel. Make sure the knee is extended (and not bent). The normal length is 45 to 55 cm. (One method of measurement is to mark the top of the head and the end of the heel on the sheet and measure between the two points).
See Newborn Assessment video for a demonstration of length measurement.
Growth Chart
Head circumference, chest circumference, length and weight are plotted on a growth chart. While in the hospital, the weight is monitored each 24 hours. After discharge from the hosital, these measurements are taken at each visit to the pediatrician to monitor growth.
Click here to plot values on an interactive growth chart. Use today's date for the birth date. Length 54 cm, weight 3.9 kg and head circumference 36 cm. Choose the newborn growth chart for a girl.
A complete head-to-toe examination follows these measurements and may be delayed until the mother has had time to breastfeed her infant or hold the infant skin-to-skin.
COMPLETE HEAD-TO-TOE SKIN ASSESSMENT
The more complete head-to-toe assessment begins with observation, listening and smell. Wear gloves if the infant has not had the first bath. Inspect the naked newborn in a well-lit, warm area. Check for skin color, rashes or birthmarks. Assess for hydration.
Skin Color
The skin color should be pink. Vernix Caseosa may be present on the skin after birth and may remain in the skin folds after the first bath. Vernix is normal. Lanugo is most noticable on the shoulders, forehead and cheeks. Acrocyanosis in the first 24 to 48 hours is normal. Ruddy or dark red color may occur with prematurity or polycythemia. Palor occurs with cardiovascular problems, blood loss or infection. Cyanosis or blue or gray color of skin or lips (circumoral cyanosis) can occur with infection, hypothermia, hypoglycemia, respiratory or cardiac difficulties. Mottled skin can occur if the infant is cold. It will resolve as the infant is warmed. Jaundice or yellowing of the skin can occur in the first days. It is usually due to high bilirubin levels from hemolysis of red blood cells. A green skin color may be due to in utero release of meconium stool by the fetus before birth. Odor may indicate an intrauterine infection.
Review the flash cards to become familiar with variations of skin assessment.
SKIN ASSESSMENT TERMINOLOGY
HEAD, NECK And SHOULDER ASSESSMENT
Assessment of the head is important as it reflects an evaluation of the central nervous system. Often assessment of the newborn's head reveals minor variations from normal which are not usually of clinical significance. Because parents often focus on the head first, it is important to reassure them of the normal variations.
Molding
Assess the appearance, shape and presence of molding.
|
|
|
|
Molding at Birth (Elsevier) |
Overriding Sutures and Molding (Dr. Janelle Aby) |
The left picture (above) shows how the head is elongated in molding. The right picture shows the angled indentation of the sutures where the bones overlap each other. This is called overriding sutures.
|
|
|
|
Cranium Molding during Vaginal Birth |
Molding After Birth and at 24 hours |
The left picture shows how the sutures allow the bones of the cranium to mold or compress to facilitate movement move through the vagina. The right picture shows the infant cranium on the first day of life and 24 hours later. Infants born via c-section birth or breech birth do not have molding. The temporary cranial asymmetry returns to a normal shape by the end of the first week.
Caput succedaneum or Cephalohematoma
With the infant lying on his back, cradle the infant's head in your hands. Feel for softness or "squishiness" on one side or both sides of the head. This can either be a "caput"(A) or a cephalohematoma (B). The swelling with caput disappears by the end of the first week whereas the swelling of cephalohematoma may take six weeks. Caput can cross over suture lines whereas cephalophematoma may be confined to one cranial bone. Neither of these variations are present with a c-section birth.
|
|
|
|
Caput Succedaneum |
Cephalohematoma (Elsevier) |



Pictures used with permission Dr. Janelle Aby, Stanford Medical School, Palo Alto, CA
The pictures above show an infant head with a caput. The first picture shows molding of the head, caput and swelling at birth. The second picture shows pitting and bruising on the head. The third picture shows an almost normally shaped head at 24 hours after birth.


Pictures used with permission Dr. Janelle Aby, Stanford Medical School, Palo Alto, CA
These pictures show a cephalohematoma. The infant has swelling over the right parietal bone (left). The right picture shows swelling over the left parietal bone.
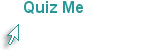
Anterior and Posterior Fontanels
While holding the head with one hand, move the "pointer finger" of the other hand to the front of the head to palpate the triangular shape of the anterior fontanel. Measure the length and the width. A rough estimate can be obtained by using the width of the finger as 1 cm and measuring the length and width in this manner. If a more exact measurement is needed, use a tape measure.
From the anterior fontanel trace your finger down the juncture of the sagittal suture and the lambdoidal suture to the posterior fontanel. This may be barely palpable. The posterior fontanel disappears at 6 weeks, whereas the anterior fontanel disappears at about 18 months. Although the anterior fontanel is described as a 5cm diamond shape, the fontanel size varies with the degree of molding. It may be difficult to palpate the fontanels if there is a great deal of molding. As the molding resolves, the fontanel size will increase. Depressed fontanels can be due to dehydration whereas bulging fontanels can be due to hemorrhage, infection or tumor. Large flat and soft fontanels could be due to hydrocephaly, hypothyroidism or malnutrition.
Neck and Shoulders
Observe the neck. Check the movement and position of the head. Restricted movement or holding the head at an angle could be due to torticollis (wryneck) or opisthotonos. Absense of head control may be due to prematurity or Down's Syndrome.
Use fingers from both hands to palpate simultaneously for intactness and crepitus of the clavicles. Assess range of motion of arms. One arm may also have decreased range of motion with clavicular fracture. This should be assessed with any difficult birth, particularly with shoulder dystocia.

This unhappy newborn has a right fractured clavicle probably due to a difficult birth with shoulder dystocia.
Picture used with permission Dr. Janelle Aby, Stanford Medical School, Palo Alto, CA
FACE: EYES, EARS, NOSE, AND MOUTH ASSESSMENT
Eyes
Most parents who see their infant for the first time focus on the head and the face especially the eyes as they are the most dominant facial feature of the neonate. Many of the worrisome abnormalities are transient phenomena, related to birth or immaturity of the neurological system.

Normal Eye
Picture used with permission Dr. Janelle Aby, Stanford Medical School, Palo Alto, CA

Conjunctival Hemorrhage
Picture used with permission Dr. Janelle Aby, Stanford Medical School, Palo Alto, CA

Pseudostrabismus
Pictures used with permission Dr. Janelle Aby, Stanford Medical School, Palo Alto, CA
An attempt to open the eyelids usually meets with resistance, especially if the infant is crying or there is a bright light. To open the eyes spontaneously, hold the infant upright and gradually rotate him. If this does not work, hold the head steady with one hand while you use the "pointer finger and thumb" of the other hand to gently open the eye and look at the iris and sclera. (See picture of "Normal eye" above). Nurses do not assess the red reflex or pupillary dilation of the newborn eye.
Ears
Assess the position of each ear by drawing an invisible line across the inner and outer canthus of the eye to the insertion of the ear, not the height of the pinna.

Normal Ear
Picture used with permission Dr. Janelle Aby, Stanford Medical School, Palo Alto, CA

Low Set Ears in Trisomy 18
Picture used with permission Dr. David Clark Stanford Medical Center, Palo Alto, CA

Preauricular Ear Tag
Picture used with permission Dr. Janelle Aby, Stanford Medical School, Palo Alto, CA
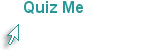
Nose
Observe for flaring (enlargement of the nostrils), a sign of respiratory distress. Newborns may do this occasionally. They may also do this more frequently after birth. If flaring occurs with an elevated respiratory rate, retractions and/or grunting, notify the physician.
Left:Normal nares Right:Flared nostrils
Malformations of the nose or copious drainage may occur with choanal atresia or congential syphillis.
Mouth
Assess the outside and inside of the mouth. The color of the lips, gums and tongue should be red.
|
|
|
|
Cleft Lip |
Cleft Palate (feeding tube is visible where palate is absent) |
Pictures used with permission Dr. Janelle Aby, Stanford Medical School, Palo Alto, CA
|
|
|
|
|
Epstein Pearls |
Bohn's Nodules |
NatalTooth |
Pictures used with permission Dr. Janelle Aby, Stanford Medical School, Palo Alto, CA
|
|
|
|
|
Normal tongue. |
Short frenulum or ankyloglossia. |
tongue after clipping short frenulum |
Pictures used with permission Dr. Janelle Aby, Stanford Medical School, Palo Alto, CA
HEART, RESPIRATORY, ABDOMEN ASSESSMENT
Heart and Respiratory
The heart and respiratory assessment were described under the initial exam and vital signs (slide 3).
|
|
|
|
Intercostal Retractions |
Subcostal Retractions |

Supernumerary Nipple Under Infant's Left Nipple
Pictures by Janelle Aby, MD, Stanford Medical School
Abdomen
Umbilical Cord
After birth, the cord is cut and clamped. Note any redness, discharge or odor which may indicate an infection. If these symptoms are present, the physician will need to be notified to determine if laboratory tests are needed.
|
|
|
|
|
Cord after birth. 2 arteries on left and one vein on right. |
Umbilical cord on Day 2 after birth. Reddness from irritation by cord. |
Umbilical cord fell off on Day 8 after birth. Normal. Monitor for drainage. |
Pictures used with permission Dr. Janelle Aby, Stanford Medical School, Palo Alto, CA
MALE AND FEMALE GENITALIA, FEMORAL PULSE ASSESSMENT
GENITOURINARY(GU) ASSESSMENT: URINE AND STOOLS
Unfasten the diaper. Always cover the penis with the diaper or you may be surprised with a shower.
Female Genitalia
The clitoris is usually edemetous. The labia majora usually covers the labia minora. In premature infants, the labia minora is prominant. In the picture below the white material is vernix caseosa. The infant may have pseudomenstruation caused by maternal hormones. This can cause a mucoid (left picture), or pink or blood-tinged discharge (diaper, right picture). There can be a vaginal skin tag. The black liquid (left picture) is the meconium, or the first stool and should be passed in the first 24-48 hours after birth. Meconium lasts 24 hours and is sticky and thick. It indicates that the anus is patent.
|
|
|
|
Female genitalia with vernix and meconium stool |
Pseudomenstruation |
Pictures used with permission Dr. Janelle Aby, Stanford Medical School, Palo Alto, CA
Male Genitalia
Observe the penis and scrotum. The picture on the left shows a normal uncircumcised male genitalia.
|
|
|
|
|
Normal term infant |
Hydrocele |
Hypospadias |
Pictures used with permission Dr. Janelle Aby, Stanford Medical School, Palo Alto, CA
Urine and stools
The first stool and urine should occur within the first 24 hours of birth. Passage of the stool usually indicates a patent anus.
|
|
|
|
|
Day 1: Large Meconium Stool |
Day 3: Large Transitional Stool |
Day 5: Small yellow stool |
Pictures used with permission Dr. Janelle Aby, Stanford Medical School, Palo Alto, CA
|
|
|
|
Very wet diaper |
Urate crystals |
Pictures used with permission Dr. Janelle Aby, Stanford Medical School, Palo Alto, CA
Diapers are very absorbent, so it is often difficult to tell if they are wet. Urate crystals are a frequent intermittent finding during the first week. It is a normal variation and needs no lab analysis.
During the first 24 hours, one wet diaper and one stooled diaper are expected. During the second 24 hours, the infant should have a minimum of 2 wet and 2 stooled diapers. After day 5, the infant should have at least six wet diapers and 2-3 stooled diapers.
At this time you may want to put a clean diaper on the infant. Remember that the designer part of the diaper is in the front and the fastening tabs are in the back. The tabs are brought to the front of the diaper can be reapplied many times. Don't forget to take off the covering over the tabs before you try to fasten them. Much easier than using cloth diapers and safety pins, but not as eco-friendly!
EXTREMITIES
REFLEXES: ROOTING, SWALLOWING, MORO, TONIC NECK, PALMAR, PLANTAR, BABINSKI, STEPPING, GALANT
Extremities
Make a general check of the extremities. Note color, symmetrical, range of motion and flexion of legs and arms.
|
|
|
|
Polydactyly |
Ligation of extra digit which falls off |
Pictures used with permission Dr. Janelle Aby, Stanford Medical School, Palo Alto, CA
Reflexes
Assessment of the reflexes determines the maturity of the neurological system. See your maternity textbook, Lowdermilk & Perry (2007), p. 653-655. Many of these reflexes are no longer evident by 4 to 6 months of age. The reflexes include the palmar grasp, sucking, rooting, swallowing, tonic neck or "fencing", moro, stepping, crawling, babinski and plantar grasp. As you become more proficient in your exam you can incorporate these reflexes in other parts of your exam.
While assessing the arms, put a finger in each of the infant's palms. The infant's fingers will curl around yours. Show the parents about their amazing newborn at the same time you do the assessment of the palmar or grasp reflex.
The sucking and swallowing reflexes are present in the term infant. They may not be present in the preterm infant. Feeding by breast or bottle cannot be initiated until the suck and swallow reflexes are present in the preterm infant.
The rooting reflex is elicited by stroking the cheek, lip or corner of the mouth. The infant turns the head toward the stimulus and opens the mouth. If close to the breast, the infant takes the nipple and begins sucking. Watch the video on how to elicit the rooting reflex.
Hold the infant in a semi-sitting position and allow the head and trunk to fall backward to an angle of at least 30 degrees. The arms will symmetrically abduct and extend while fanning the fingers to form a C with thumb and forefinger. Legs follow a similar pattern. A tremor may be seen. (The infant is not shivering). This is the moro reflex. While you have done other parts of the exam, you may have already noticed the infant throw his/her arms out in response to jarring the the bed or a loud laugh. This is sufficient to assess the reflex.

Moro Reflex (Elsevier)
Watch two videos on how parents have elicited the Moro Reflex:
The tonic neck or fencing reflex is seen by turning the head gently to one side while the infant is falling asleep or sleeping. With the face looking to the left, the left arm and the left leg will be extended. The right arm and leg will be flexed. Turn the face to the right and the right leg and arm will be extended and the left arm and leg will be flexed. Watch the short video about what the tonic neck reflex looks like.
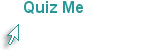
The plantar reflex is elicited by pressing your finger at the base of the toes. The toes curl around your fingers.
Babinski reflex is elicited by moving your finger on the side of the foot from the heal across the the ball of the foot. A positive babinski is normal in newborns when all toes hyperextend with dorsiflexion of the big toe. Click here to view a babinski reflex.
Babinski Reflex (Elsevier)
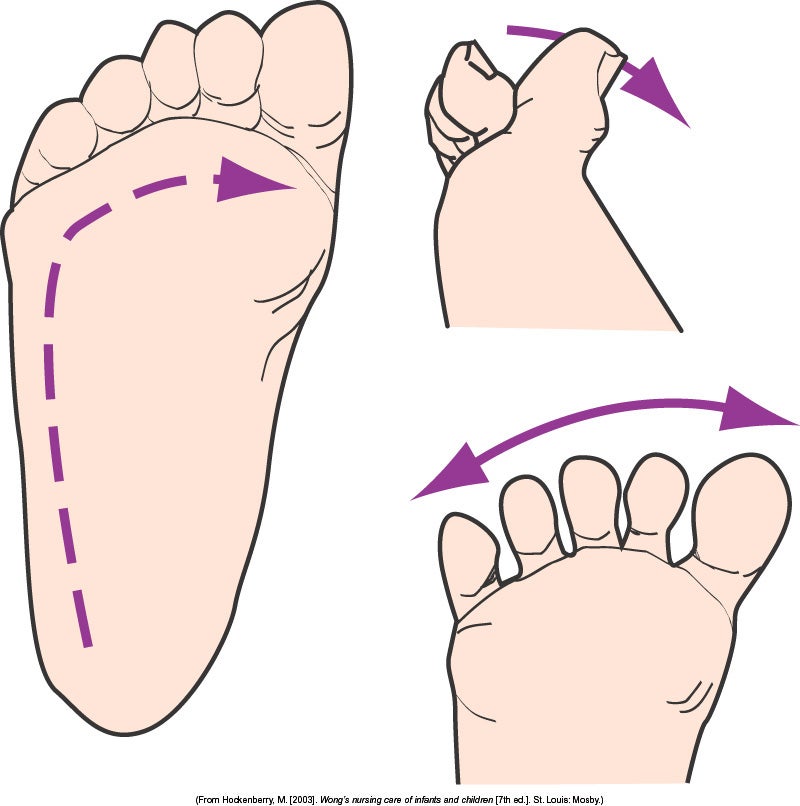
The stepping reflex can be elicited by holding the infant vertically, allowing one foot to touch the table and then the other. Click here to view a video of the stepping reflex.
Stepping Reflex (Elsevier)
Galant or trunk incurvation is seen when the infant is placed prone. Run the finger down the back lateral to the spine. The trunk will swing toward the stimulted side. Watch the movie to learn how to elicit the Galant reflex.
For additional video clips of the reflexes please click here.
BACK, SPINE, ANUS
Support the infant's head when you turn it from back to stomach. Put one hand behind the head and slip the other hand/arm under the infant's chin and stomach and turn over. Let the infant lie on his/her stomach (with legs pulled up). Use the same method to turn the infant from front to back.
The infant may be able to lift the head momentarily.
Inspect the spine and shoulders for straightness and flexibility. Check the base of the spine for a pigmented nevus with a tuft of hair. The infant may have a pilonidal dimple, a small dimple at the base of the spine without connection to the spinal cord. This is often associated with spina bifida occulta.
|
|
|
|
|
Sacral Dimple |
Stretching spinal dimple to make sure the base is intact. |
Meningomyelocele-an external sac containing meninges and cerebrospinal fluid. |
Pictures used with permission Dr. Janelle Aby, Stanford Medical School, Palo Alto, CA
This is a good time to elicit the Galant reflex and check for Mongolian or Slate-grey spots. Check that there is one anus. Passage of a meconium stool either in utero or within the first 24 hours of birth signifies a patent anus. Rectal temperature is no longer used to check for anal patency. When you have completed the exam, turn the infant to the back, make sure the diaper is clean and fastened. Redress the infant. This is a good time to ask the parents if they want you to show them how to wrap the baby. First time parents and the father are usually interested in this education. Review parental education on handling and sleep patterns (see sidebar).
CONGRATULATIONS!
YOU HAVE COMPLETED THE NEWBORN ASSESSMENT eLEARNING MODULE!
GO TO THE ASU ONLINE LEARNING RESOURCE CENTER TO WATCH THE FOLLOWING NEWBORN ASSESSMENT Videos.
Newborn Physical Assessment Video
Gestational Age Assessment Video